Lymph Nod Cancerv About
Source(google.com.pk)Some of the most important advances in cancer have to do with stopping excess treatment that is not helping, and may be harming patients. Yet, this is often the type of advance that is slowest to take hold, because psychologically and economically, there is much more momentum for trying new treatments that will be profitable than to stop treatments that have been shown to no longer be effective.
Breast cancer is the most common cancer for women, and breast cancer research has more funding than other cancers. Thus, we are farther ahead in our way of thinking about breast cancer treatment (and analogously for men, prostate cancer treatment) than we are about other cancers. We are witnessing a change in the culture of cancer that is long overdue.
The cancer culture has a lot of inertia. Some of this is a natural consequence of doctors learning current dogma during their training and being resistant to change that a decade or two later. I have not attended medical school, but I suspect that schools could do a better job of reminding their trainees that current medical treatments should never attain hallowed status because our knowledge changes so rapidly. Breast cancer has a long history of this – for example, radical mastectomies are now rare, because they have been shown most of the time not to extend the lives of women with breast cancer, and they are often detrimental to quality of life.
We are at a new surgical turning point. A recent study by Giuliano et al. (2011) took on the currently standard protocol of axillary node dissection surgery after finding a positive lymph node during initial lumpectomy and sentinel lymph node analysis. This result will positively affect the quality of life of many thousands of women.
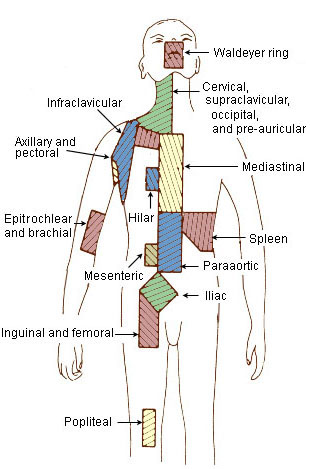
Axillary lymph nodes
Axillary lymph nodes
Translation and history:
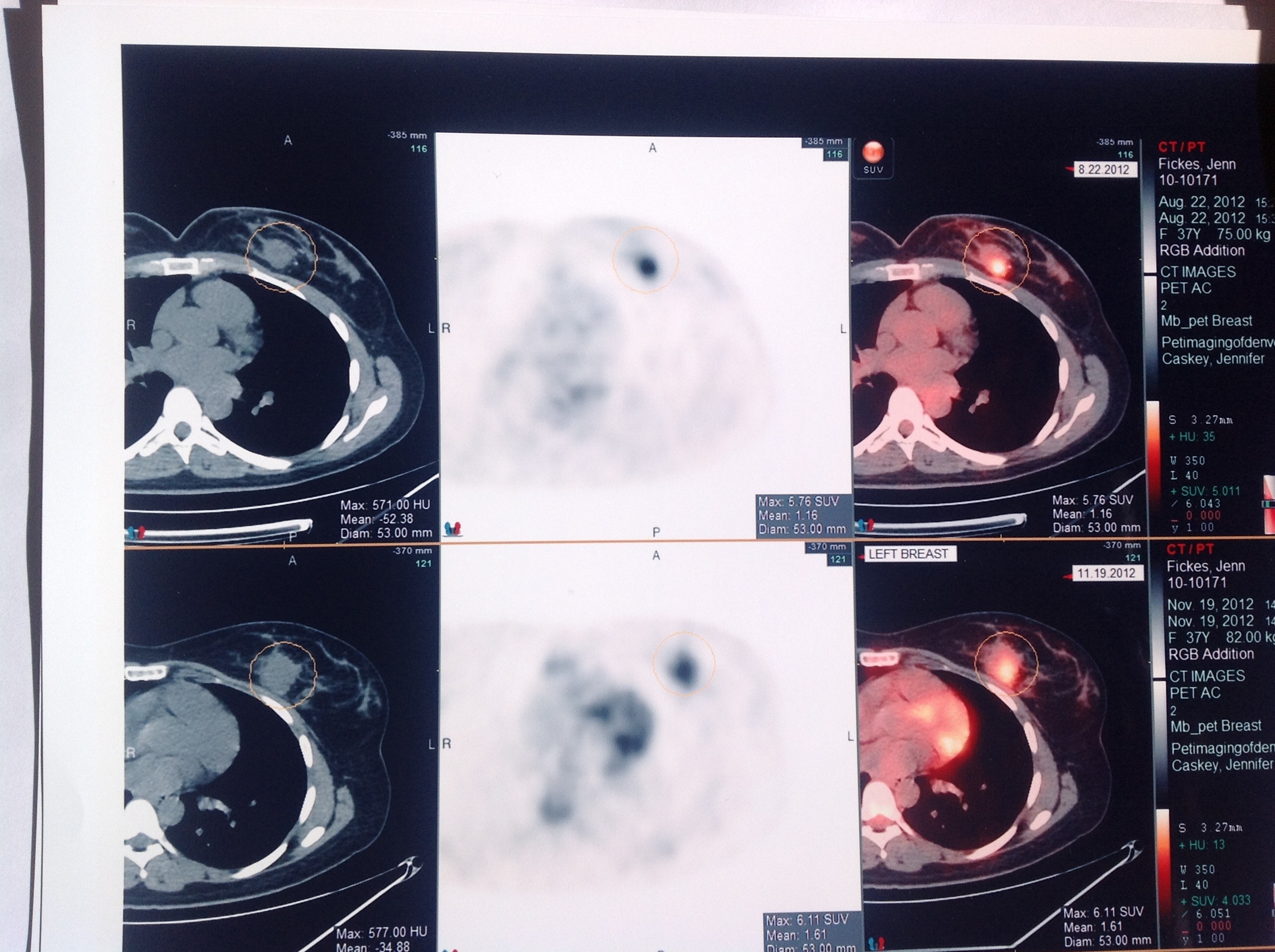
The first place that breast cancers metastasize is in the axillary (armpit) lymph nodes. Just as surgeons used to think that the pectoral muscle must be removed with the breast during a mastectomy (=radical mastectomy), current dogma is that lymph nodes with tumors should actively found and removed, in a surgery called axillary lymph node dissection (ALND). Cancer doctors have differed on whether or not the value of this is merely diagnostic (just finding out how far cancer has spread) versus also therapeutic (getting potentially dangerous cancer cells out of the body) – but there was widespread agreement that the value was there. Even if we believe only in diagnostic value, current scanning technology cannot detect the smallest tumors (under about half a centimeter). The only method currently available for thoroughly checking lymph nodes is permanent surgical removal. This means that many (probably most) women who have ALND surgery end up finding out that the surgery was not necessary, because all the lymph nodes removed were negative.
Though for some this procedure might seem worth it to set the mind more at ease, it can have quality-of-life implications. Anyone who has had this surgery is handed a leaflet afterwards with instructions about caring for her now lymph-node deprived arm. Because lymph nodes are involved in fluid balance in the body and the immune system, there is some risk for these women that they will develop swelling in their affected arm at times (called lymphedema), and/or infections from wounds.
The level of risk for these complications is poorly understood. The problem is, there have been very few studies to determine what women should do to lower their risk for lymphedema and infections. If you have had ALND, very recent studies suggest strongly that some of the instructions given to you by your doctor have the potential to increase risk for lymphedema.
What’s clear, though, is that having fewer lymph nodes does increase these risks by some finite amount. ALND surgery also cuts a lot of nerve endings, so large areas of the shoulder and arm become numb, permanently for most people.
Because of this morbidity (risk for other health problems) associated with ALND, a brilliant protocol was developed over the last decade or so in which surgeons avoided taking out more lymph nodes than necessary. In sentinel lymph node dissection (SLND), surgeons use a dye injected near a tumor to determine which lymph nodes drain directly from the tumor. If the first node (or first few) is removed in surgery and determined to be cancer-free, the probability that further lymph nodes contain cancer is very low, and those patients are handed a get-out-of-ALND-free card.
But, those patients who have a positive sentinel lymph node are told that they must undergo an ALND to determine the current extent of lymph node spread, and remove any cancer in further nodes to help reduce its spread in the future. This rationale seems perfectly logical; the problem is that there has never been any science to support it. (In fact, there were some early papers that found no difference in survival between positive SLND patients who underwent ALND and those who did not [including Fant et al. 2003; Naik et al. 2004; Jeruss et al 2005; Hwang et al. 2007]. The major caveats with these studies though were first, that the procedure was so new that women could only be followed for a few years; and second, that the groups were not randomized, and women were allowed to choose which group to be in. This leads to an obvious bias that those choosing not to undergo ALND were those with a better prognosis in the first place.)
Finally, we have a randomized trial (in which patients do not get to choose whether or not to have the procedure) that confirms the results from the previous papers. That is, it’s looking more and more as though even women with a positive lymph node from SLND do not need follow-up ALND. Because SLND involves removing far fewer lymph nodes than ALND (in the study, a median of 2 nodes removed vs. 17, respectively) there is far lower risk for subsequent arm problems affecting quality of life for breast cancer patients. This is no small consideration, now that so many women with breast cancer are living cancer-symptom-free for decades after treatment (the 5-year survival rates in the study were over 90% for both treatment groups, and the 5-year disease-free rates were both over 80%). There were significantly more lymphedema and significantly higher infection rates in the ALND group than in the SLND group.
What about the women who underwent ALND and more positive lymph nodes were found? Didn’t having them removed help protect them from recurrences later? Apparently not, if they were already having hormone therapy, radiation treatment and/or chemotherapy. That’s because the treatments are redundant – nonsurgical treatments have been effective enough in destroying remaining cancer cells in the lymph nodes.
The caveat presented in the study was that because it involved lumpectomy patients, the results are not extensible to women who undergo mastectomies. But because treatment outcomes for mastectomy are the same as for lumpectomy with radiation, it is highly likely that subsequent analogous studies using mastectomy patients will have similar results.
The long and the short of this is that patients need to continue to be proactive about their treatment. They should respect their doctor’s expertise, but also not to be afraid to ask questions, such as whether or not their doctor believes this study applies to them, because doctors are often slow to drop treatments that they have believed for years or decades to have been effective; doing so admits that they have been overtreating patients and potentially causing some suffering. They should not feel guilt. They were making the best choice they could based on the information they had, and non-surgical treatments are more powerful now than they used to be, so there may have been a time when ALND actually did have therapeutic value. The problem is that we are extremely biased in what research gets funded and what doesn’t; and testing current treatment standards takes a huge backseat to testing new drugs, because so much research funding comes from pharmaceutical companies.
As a disclosure, I had ALND surgery in 2008 after a positive node was removed during SLND and based on my reading of the older papers, did not believe I needed ALND. Furthermore, a calculator available on the Sloan-Kettering site predicted the probability of additional positive lymph nodes for someone with my pathology to be about 17%. But on strong advice from my surgeon and most importantly on advice of one of the authors of some of the older studies showing no benefit to ALND, I went ahead with the surgery (I speculate that that author might now give different advice; but it is understandable that doctors feel the need to be conservative and often recommend stronger treatment than is probably necessary).
I have not yet had any serious complications from the procedure, but they could become more likely as I grow older. From the start, however, I have followed the recommendations for preventing lymphedema based on science, not the leaflet from the surgeon’s office, and if you have had ALND surgery, you should discuss the recent findings with your own doctor. (I found that my surgeon was willing to admit to me that his office’s instructions were not based on any known science, and he even told me straight out not to follow some of the recommendations. But he still gave me the inaccurate leaflet to take home with me.)
References
Fant JS, Grant MD, Knox SM, Livingston SA, Ridl K, Jones RC, Kuhn JA, 2003. Preliminary outcome analysis in patients with breast cancer and a positive sentinel lymph node who declined axillary dissection. Ann Surg Oncol. 10(2):126-30.
Giuliano AE, Hunt KK, Ballman KV, Beitsch PD, Whitworth PW, Blumencranz PW, Leitch AM, Saha S, McCall LM, Morrow M., 2011. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA 305(6):569-75.
Hwang RF, Gonzalez-Angulo AM, Yi M, Buchholz TA, Meric-Bernstam F, Kuerer HM, Babiera GV, Tereffe W, Liu DD, Hunt KK, 2007. Low locoregional failure rates in selected breast cancer patients with tumor-positive sentinel lymph nodes who do not undergo completion axillary dissection. Cancer. 110(4):723-30.
Jeruss JS, Winchester DJ, Sener SF, Brinkmann EM, Bilimoria MM, Barrera E Jr, Alwawi E, Nickolov A, Schermerhorn GM, Winchester DJ, 2005. Axillary recurrence after sentinel node biopsy. Ann Surg Oncol. 12(1):34-40.
Naik AM, Fey J, Gemignani M, Heerdt A, Montgomery L, Petrek J, Port E, Sacchini V, Sclafani L, VanZee K, Wagman R, Borgen PI, Cody HS 3rd, 2004. The risk of axillary relapse after sentinel lymph node biopsy for breast cancer is comparable with that of axillary lymph node dissection: a follow-up study of 4008 procedures. Ann Surg. 240(3):462-8; discussion 468-71.
Lymph Nod Cancerv
Sign Ribbon cells Horoscope Symbol Tattoos Research Zodiac Sign Ribbon Tattoos

Lymph Nod Cancerv
Sign Ribbon cells Horoscope Symbol Tattoos Research Zodiac Sign Ribbon Tattoos

Lymph Nod Cancerv
Sign Ribbon cells Horoscope Symbol Tattoos Research Zodiac Sign Ribbon Tattoos

Lymph Nod Cancerv
Sign Ribbon cells Horoscope Symbol Tattoos Research Zodiac Sign Ribbon Tattoos

Lymph Nod Cancerv
Sign Ribbon cells Horoscope Symbol Tattoos Research Zodiac Sign Ribbon Tattoos

Lymph Nod Cancerv
Sign Ribbon cells Horoscope Symbol Tattoos Research Zodiac Sign Ribbon Tattoos

Lymph Nod Cancerv
Sign Ribbon cells Horoscope Symbol Tattoos Research Zodiac Sign Ribbon Tattoos

Lymph Nod Cancerv
Sign Ribbon cells Horoscope Symbol Tattoos Research Zodiac Sign Ribbon Tattoos
Lymph Nod Cancerv
Sign Ribbon cells Horoscope Symbol Tattoos Research Zodiac Sign Ribbon Tattoos
Lymph Nod Cancerv
Sign Ribbon cells Horoscope Symbol Tattoos Research Zodiac Sign Ribbon Tattoos

No comments:
Post a Comment